Digital Pathology: What Every CIO Needs to Know

by Patrick Myles
CEO, PathPresenter

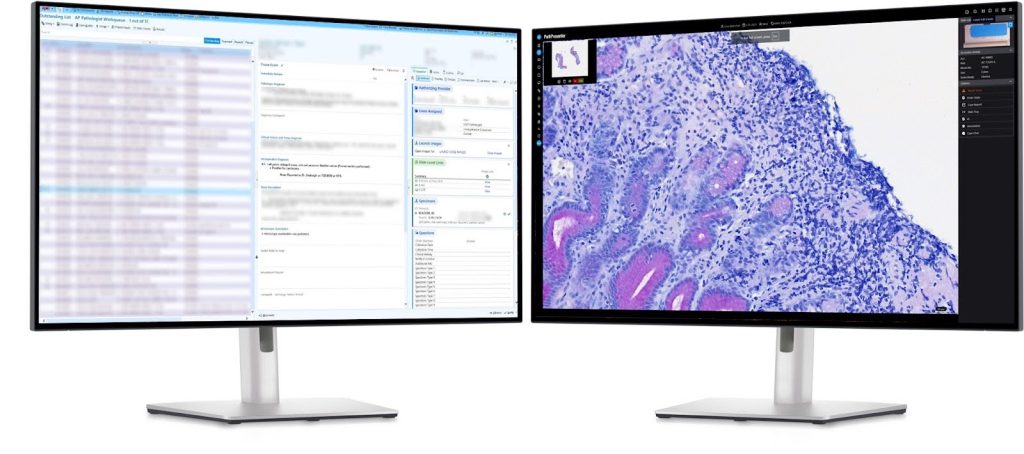
As healthcare systems embrace digital transformation, digital pathology is becoming a cornerstone of precision medicine. By digitizing glass slides into high-resolution images and integrating them into clinical, education, and research workflows, hospitals and laboratories can reap the many benefits of new digital tools in pathology, including access to promising new AI algorithms. However, the transition to digital pathology presents a complex set of IT challenges and requirements, particularly for CIOs responsible for ensuring operational readiness, scalability, security, and compliance.
This article outlines key technical considerations for digital pathology workflow systems with insights earned from the experience of real-world implementations.
Digital Pathology: Growing Pains

For CIOs familiar with enterprise imaging and PACS, it’s important to understand that digital pathology presents distinct challenges. Enterprise imaging has reached a level of maturity where standardized protocols—most notably DICOM—are widely adopted, enabling consistent image formatting, storage, and interoperability across systems. In contrast, digital pathology is still in the early stages of standardization. Key components of the digital pathology workflow—such as slide scanners, laboratory information systems (LIS), image management systems (IMS), and AI tools—often operate in silos with limited interoperability. While concepts from PACS remain relevant to pathology, and emerging standards like DICOM for pathology are beginning to bridge the gap, the digital pathology field is still in the process of catching up to the more unified and standardized environment found in enterprise imaging.
As a result, there is no “one size fits all” cookie cutter solution for a digital pathology project. Each institution is unique and so are their implementations of digital pathology. Hidden complexities often arise mid-process, requiring flexibility and expertise from the vendors and development teams. Implementing digital pathology requires addressing a multitude of complex technical and operational challenges, underscoring the importance of a well-planned and executed strategy.
IT Challenges in Digital Pathology
Multiple scanners and slide formats

The slide scanning market has a variety of vendors, many with their own proprietary file formats for whole slide images (WSI). These include Leica’s .SVS format, Hamamatsu’s .NDPI, Philips’s .TIFF variant, 3DHISTECH’s .MXRS, Roche’s .BIF, Evident’s .VSI and more. Broad format support and interoperability are important factors of selection for the IMS and LIS platforms that will manage the slide images.
Additionally, a fully featured IMS should support not just whole slide images but gross (macroscopic) images, clinical photographs, radiology images (e.g. DICOM format), molecular and genomic visualizations, cytology images, documents and reports, and even video. Therefore the image management system plays a key role as a central hub providing the access that unlocks the full value of these various imaging assets.
Storage and Performance – The Elephant in the Room

Storage is the elephant in the room: digital pathology generates huge, multi-gigabyte images, and IT must deliver fast transfer and rendering to give pathologists microscope-like responsiveness—while balancing performance, scalability, security, budget, and compliance.
On-Premise Architectures
Strong on security, data sovereignty, and low-latency performance, but costly to build, maintain, and scale; large images can strain local networks and expose legacy limitations.
Cloud Architectures
Highly scalable with built-in redundancy and lower IT burden, but offers less direct control over data, more complex regulatory considerations, and potential vendor lock-in.
Hybrid Architectures
Keeps active data on-prem for speed and uses the cloud for archival storage, balancing cost and control. The tradeoff is added complexity in synchronizing, securing, and monitoring two environments.
Performance Considerations
Serving hundreds of users requires high-bandwidth networks and efficient image streaming (like Google Maps tiles), often supplemented by GPU-accelerated resources or HPC clusters for AI. CDNs or edge caches help further reduce latency.
LIS Integration
Lab information systems such as those from EPIC, Novopath, and LigoLab are vital to managing, tracking and documenting diagnostic workflows in pathology, and so a smooth integration between LIS and IMS is key to system level usability and effectiveness. Not all LIS (particularly legacy systems) were built for wider digital pathology workflows and many lack built-in support for two-way communication and AI integration. Even within one LIS platform, different versions can prevent easy integration. The market has multiple approaches and protocols for integration (e.g. HL7, TCP/IP, SFTP, HTTPs, VPN) and multiple interface engines (e.g. Mirth, Rhapsody). Integration is key to unlocking the benefits of digital pathology, so systems not built with integration in mind can face significant obstacles or complexity in customization and workarounds.
AI Model Integration
As in enterprise imaging, AI is playing an important role in advancing pathology, offering previously unseen capabilities that are driving precision medicine. But with that power comes complexity, especially when integrating with other system components. Some AI models, especially the earliest, have been designed as purely standalone with no workflow integration to an IMS or LIS. Ideally, AI functionality should be easily accessible from the LIS or IMS, and the output of AI analysis models should flow seamlessly back into the larger network of systems to be available across the entire workflow.
Another challenge comes from the different ways various AI models work: some operate on patches (specific sub-regions of an image), some with whole slides, textual data, or a combination. Developers may have built their own viewers specifically for their models to optimize their use, but since pathologists will often seek to use multiple tools to address different specialties, a unified viewer (available in some IMSs) that integrates multiple models simplifies the user experience and minimizes errors or inconsistencies from switching between different systems.
AI brings its own infrastructure considerations too. AI implemented on-prem has fewer security issues since data does not leave the organization’s environment and data transfer and processing are local, but some AI vendors are not comfortable placing their algorithm code on-prem. On-prem also requires a heavy compute infrastructure with the associated maintenance and support personnel. Cloud once again offers scalability and flexibility with lower infrastructure requirements and no intellectual property concerns for AI vendors, but it trades that against issues of data transfer bandwidth, security, cost, regulatory compliance and data sovereignty.
Security considerations

It goes without saying that security for personal health information (PHI) must be paramount (and regulated). This requires end to end encryption for all data transfer between LIS, IMS, and AI models, as well as robust user authentication, role based access control, and comprehensive audit trails logging the complete history of all data interactions.
Choosing the Right Workflow/IMS Partner

Implementing digital pathology is a complex and specialized endeavor, requiring more than just good technology—it demands the right partner. While no two deployments are alike, many institutions have already paved the way with successful implementations. Their secret? Choosing vendors with deep expertise in both pathology workflows and the underlying IT infrastructure. A seasoned partner brings not only technical solutions but also real-world insight from integrating diverse systems at scale. Flexibility, scalability, and a strong understanding of clinical requirements are key to navigating this transformation smoothly.
Final Thoughts for Leaders
Implementing a digital pathology workflow is a strategic, multidisciplinary undertaking that sits at the intersection of IT, diagnostics, and data governance. It often involves intricate, hidden challenges. CIOs play a pivotal role in orchestrating the infrastructure that enables seamless slide digitization, secure data access, AI readiness, and EHR interoperability—all under the umbrella of compliance and performance. With thoughtful architecture and careful vendor selection, digital pathology becomes not just a technology shift, but a transformative enabler of modern, connected, and data-driven healthcare.
About the Author
Patrick Myles is CEO of PathPresenter, a global digital pathology workflow platform. With prior leadership roles at Huron Digital Pathology and Teledyne DALSA, he drives innovation in image management, AI and healthcare IT. He holds an MBA from Wilfrid Laurier University.
More Posts
- Behind the Scenes of a Successful FDA 510(k): PathPresenter’s Clinical Viewer Journey
- The Digital Pathology Illusion: Why Are We Building Storage Instead of Solutions?
- Success Story: Accelerating Clinical Trials for Oncology with Imagenomix Predict and PathPresenter ConsultConnect
- Why Seamless IMS-LIS Integration Is Essential for Digital Pathology
- Digital Pathology Basics: Image Viewers vs. Image Management Systems
